Emergencies can arise unexpectedly, and when it comes to dental issues in children, swift and appropriate action is paramount. In this comprehensive guide, we’ll delve into essential information for parents concerning emergency dental care in child-friendly dentistry environments. Through this concise yet informative guide, you’ll learn how to respond promptly in the event of a dental emergency involving your child.
Recognizing Dental Emergencies for Kids
Common dental emergencies children may encounter include:
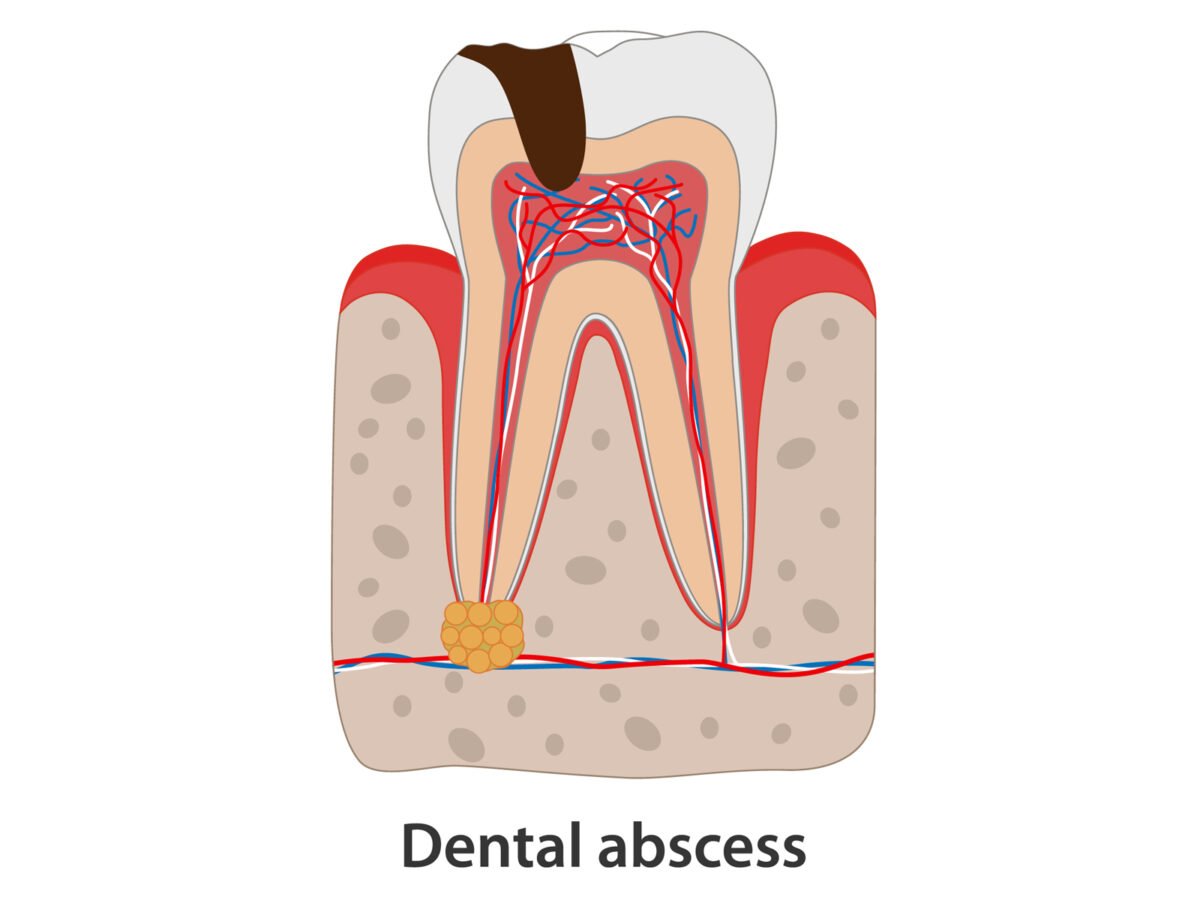
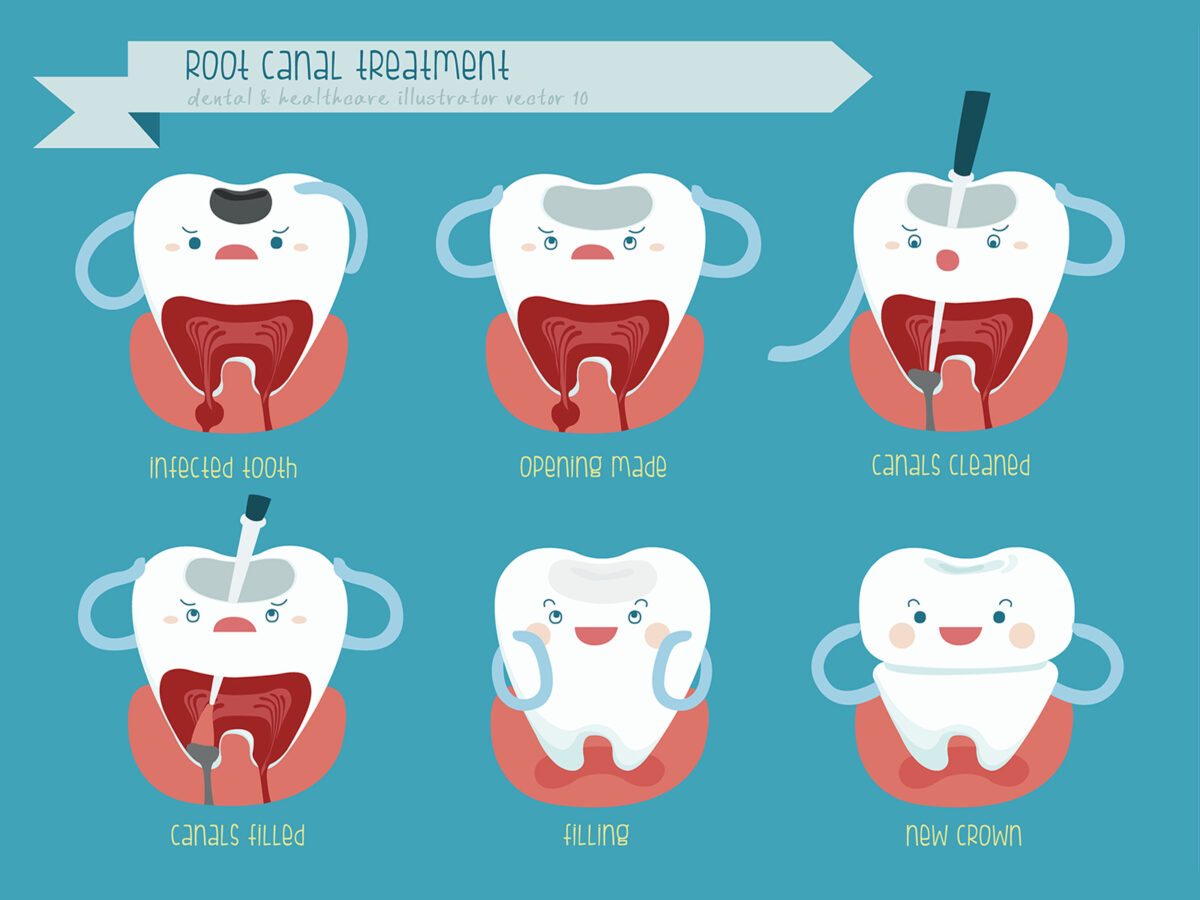
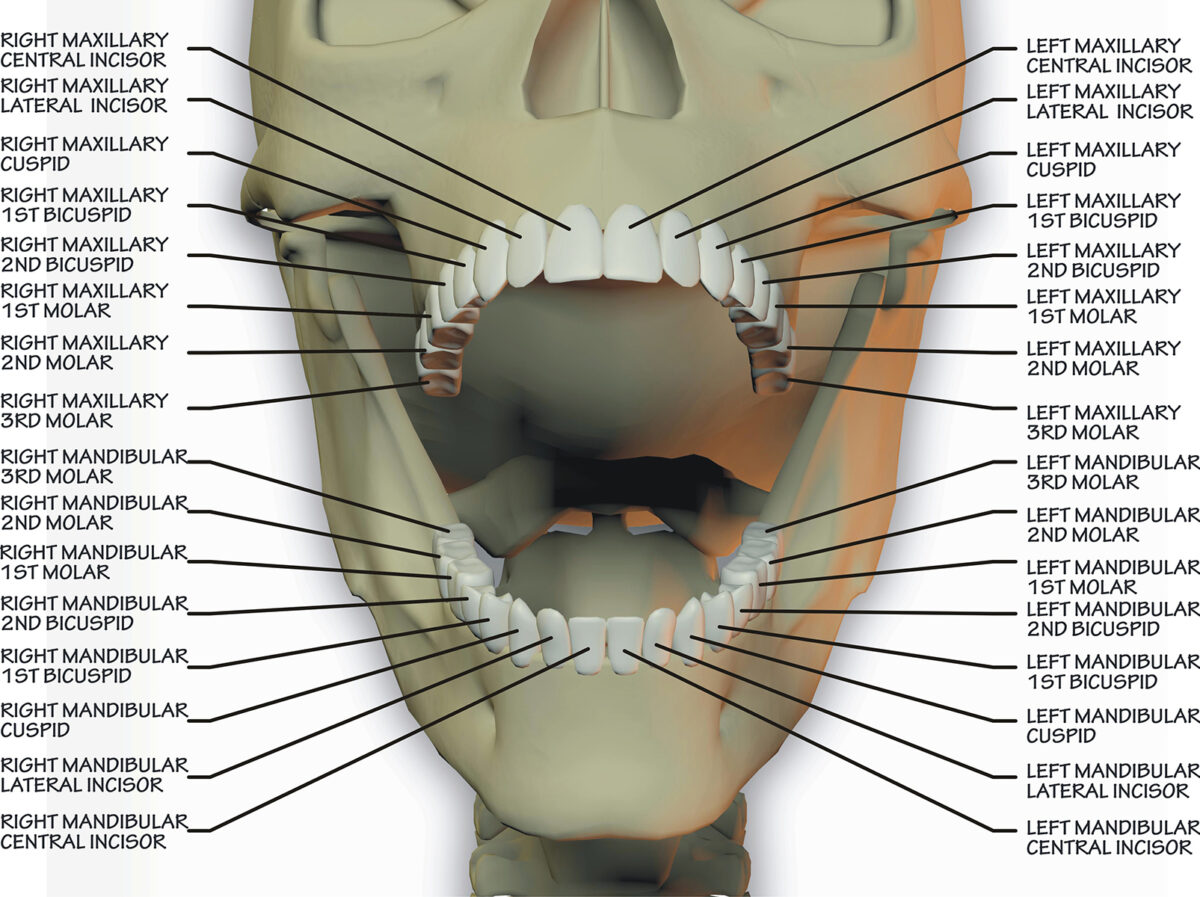
- Toothaches: Persistent or severe toothaches may indicate underlying issues like decay, infection, or trauma.
- Knocked-Out Teeth: Prompt action is crucial if a child’s tooth is knocked out. Preserve the tooth in milk or saliva and seek immediate dental attention.
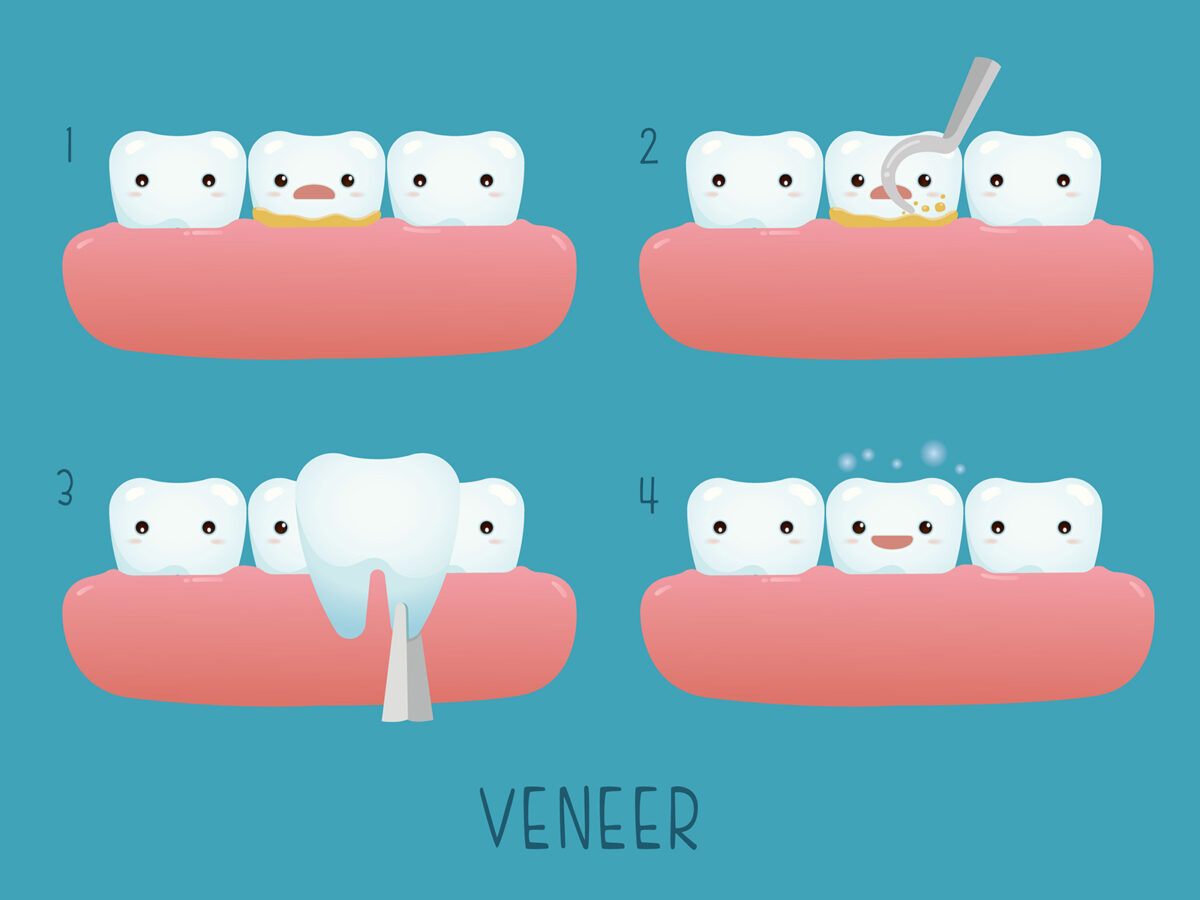
- Broken or Chipped Teeth: Fractured teeth require prompt assessment by a dentist to prevent further damage or infection.
- Loose or Displaced Teeth: Trauma or injury can cause teeth to become loose or misaligned, necessitating dental evaluation to prevent complications.
Immediate Steps for Parents in Child-Friendly Dentistry Emergencies
Parents can take simple yet crucial actions during a dental emergency involving their child:
- Stay Calm: Reassure your child and maintain composure to ease anxiety.
- Assess the Situation: Gauge the severity of the dental issue and provide immediate first aid if necessary.
- Contact the Dentist: Reach out to your child’s dentist or pediatric dentist for guidance and to arrange an emergency appointment.
- Manage Pain: Administer over-the-counter pain relief medication as directed and apply a cold compress to alleviate swelling.
- Preserve Teeth: Preserve any knocked-out teeth in milk or saliva until you can consult the dentist.
Essential Considerations in Child-Friendly Dentistry Emergencies
When dealing with a dental emergency involving your child, keep these considerations in mind:
- Comforting Environment: Child-friendly dental offices are designed to create a welcoming and reassuring atmosphere for young patients, helping alleviate fear and anxiety.
- Pediatric Expertise: Pediatric dentists specialize in addressing children’s dental needs, including emergencies, and are equipped to handle a wide range of dental issues in young patients.
- Gentle Approach: Child-friendly dentists employ gentle techniques and age-appropriate communication to interact with children, ensuring a positive experience.
- Parental Involvement: Parents are encouraged to actively participate in their child’s dental care, especially during emergencies, with child-friendly dentists offering guidance and support throughout the process.
Preventing Dental Emergencies for Kids
To minimize the risk of dental emergencies in children, consider the following preventive measures:
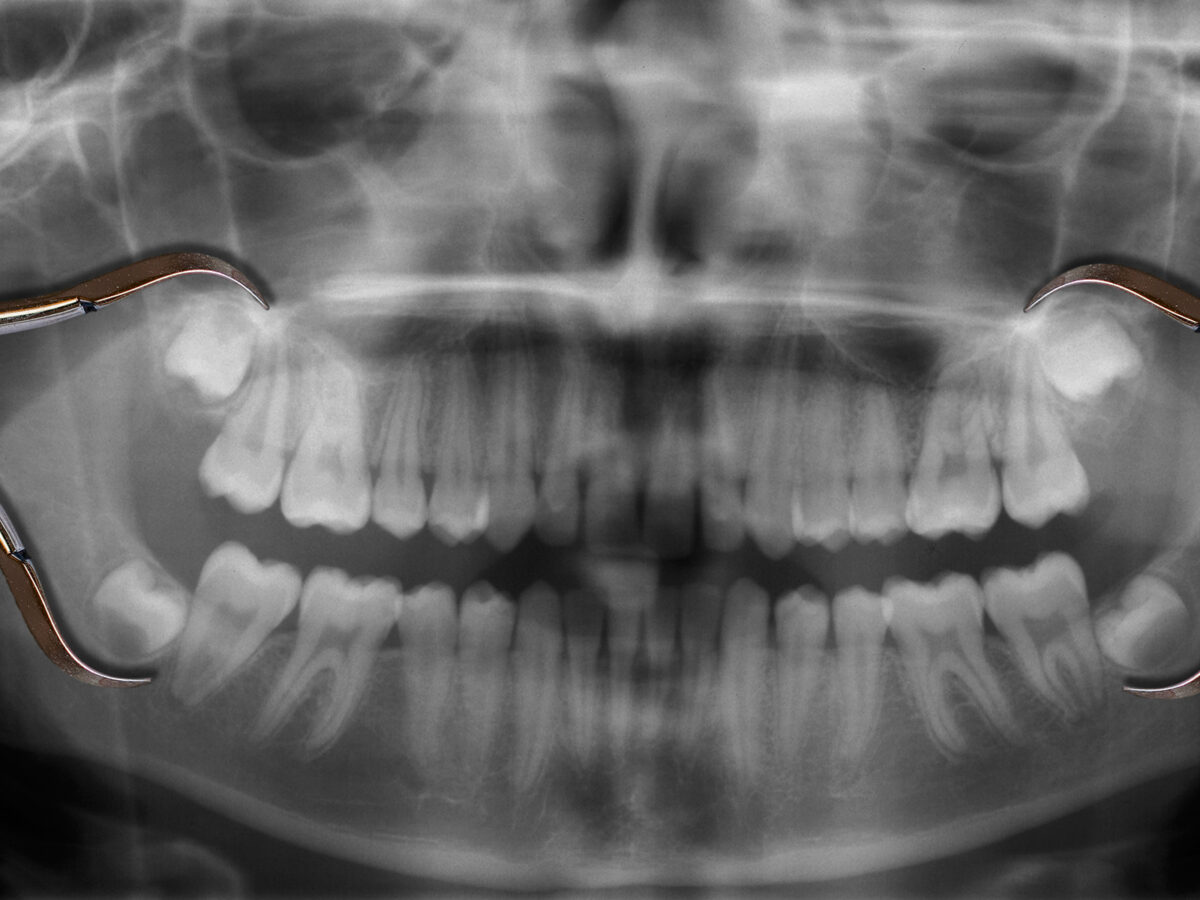
- Regular Dental Visits: Schedule routine dental check-ups for your child to detect and address potential issues early on.
- Protective Gear: Encourage the use of mouthguards during sports and physical activities to prevent dental injuries.
- Healthy Habits: Teach your child good oral hygiene practices, including brushing twice daily, flossing, and maintaining a balanced diet for optimal oral health.
Conclusion
Emergency dental care for children necessitates prompt action and specialized attention. By promptly recognizing dental emergencies, knowing how to respond effectively, and seeking care from child-friendly dentistry providers, parents can ensure the best possible outcome for their child’s oral health. Prioritizing preventive measures and regular dental visits will help minimize the risk of emergencies and keep your child’s smile healthy and vibrant.